V
O
B
The Problem
Benefits verification is slow, inconsistent, and expensive.
Most teams do VOB by phone calls, portal scraping, or brittle integrations. Even when you can fetch a 271, the output isn't operational: it's hard to interpret, hard to trust, and it doesn't update your system.
See How We Solve This





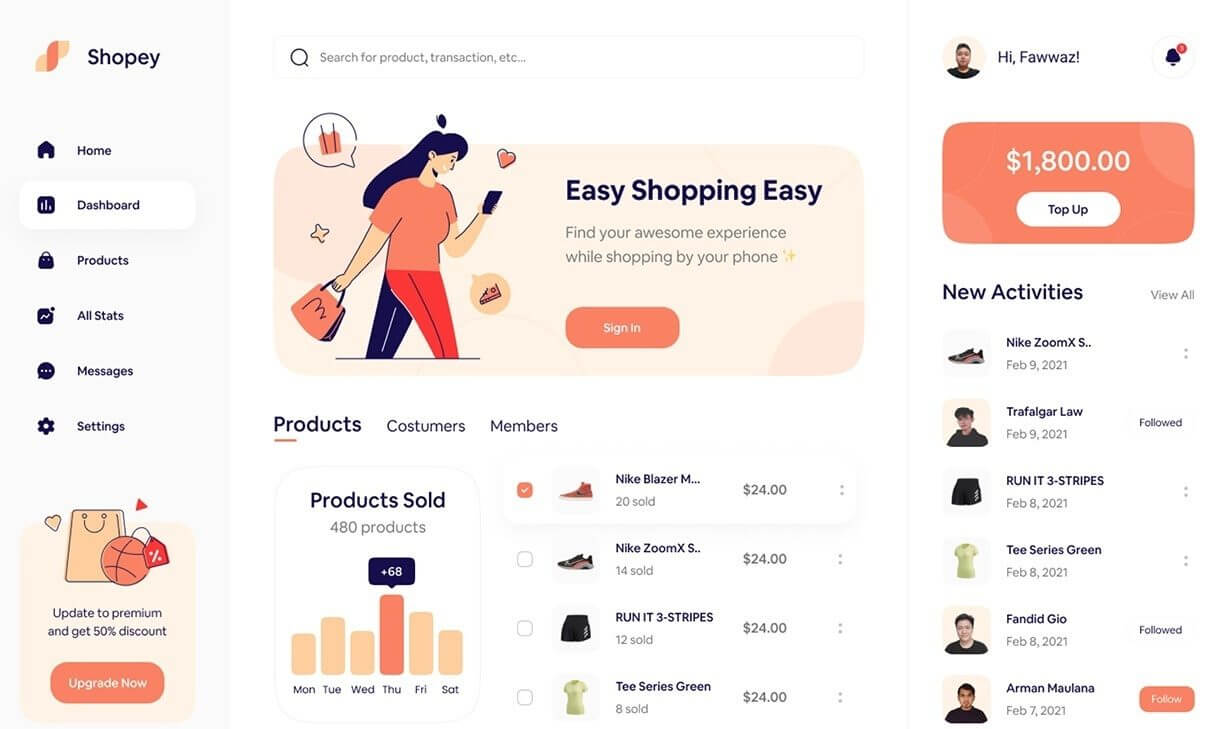
One check in. A decision out.
Instead of "here's a raw eligibility response," you get: ACCEPT / NEEDS INFO / DENY, with reasons and next actions.
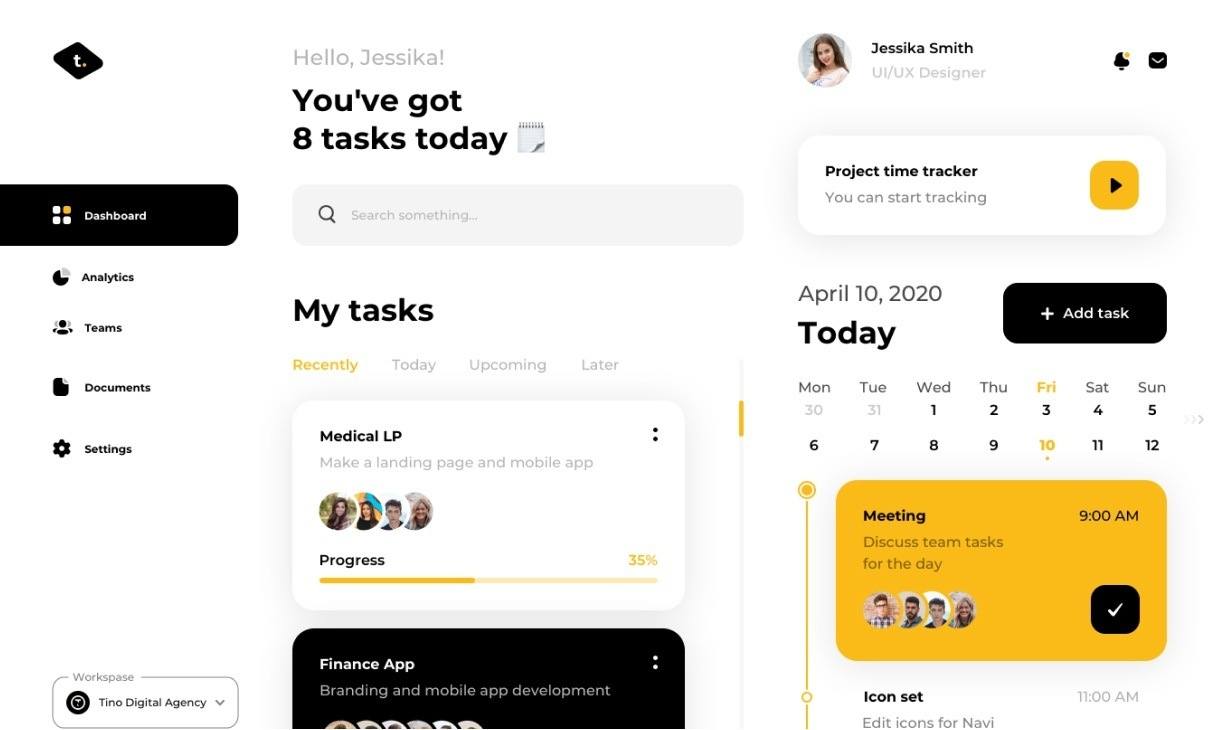
The Decision Object
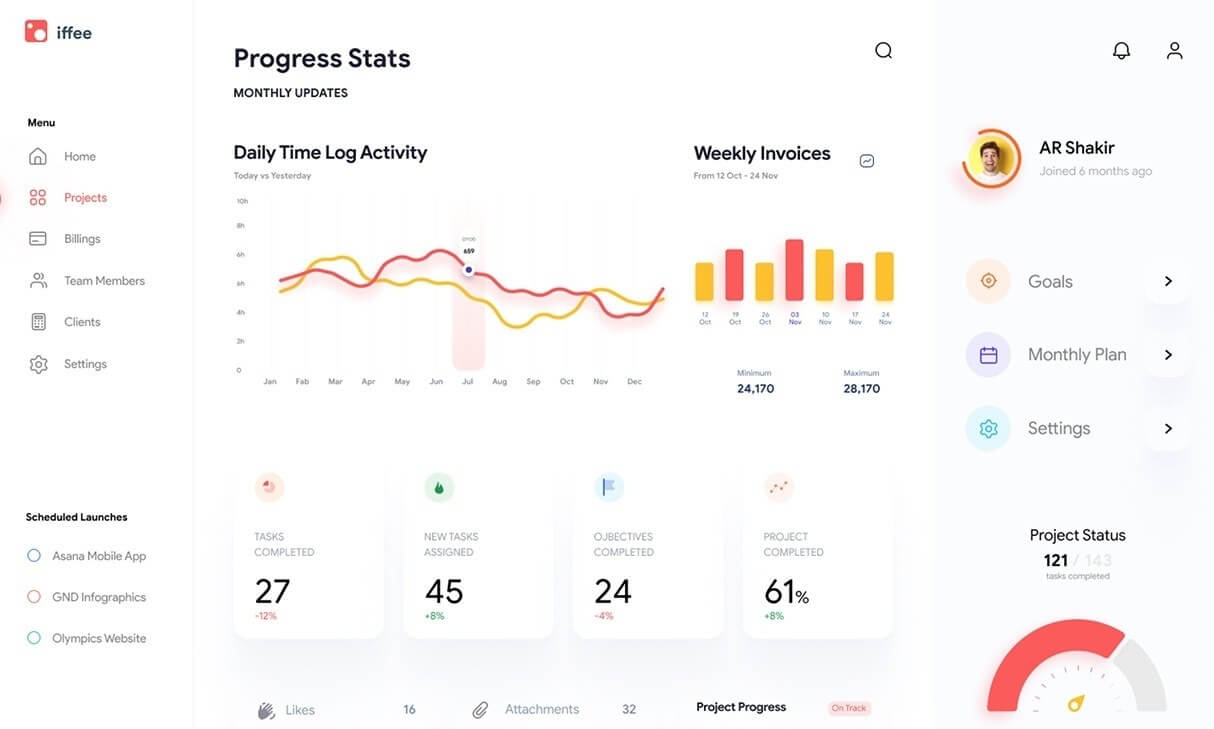
Built for operations —not just data.
Every response includes coverage status, decision (ACCEPT | NEEDS_INFO | DENY), reasons, confidence score, and recommended actions. Your team sees the same answer every time, no matter the payer.
View API DocsTrusted by healthcare organizations.





Pricing Plans
Simple, transparent pricing.
API Plan
Usage
For Developers
- Send documents for eSigning
- Multiple User
- Refund
- Bulk invite to sign
Automation Plan
Custom
For Operational Teams
- Send documents for eSigning
- Multiple User
- Refund
- Bulk invite to sign
Clinic Plan
Bundled
For Small Practices
- Send documents for eSigning
- Multiple User
- Refund
- Bulk invite to sign
Silver Plan
$123
Great for Individial Person
- Send documents for eSigning
- Multiple User
- Refund
- Bulk invite to sign
Gold Plan
$199
Great for Startup
- Send documents for eSigning
- Multiple User
- Refund
- Bulk invite to sign
Business Plan
$239
Great for Large Business
- Send documents for eSigning
- Multiple User
- Refund
- Bulk invite to sign








